Patients with end-stage respiratory conditions like lung cancer, COPD, emphysema, and other pulmonary issues often have an unpredictable disease progression, making prognosis difficult for patients, caregivers, and healthcare professionals alike. Lung conditions frequently fluctuate with intermittent crisis episodes or hospitalizations followed by repeated periods of recovery. As a result, hospice care is often delayed and its benefits underutilized.
“Having end-of-life conversations and planning is vital because lung conditions can take years to decline with a seemingly rapid end stage,” said Heather Lumsdon, CNO with Heart to Heart Hospice. It’s hard to pinpoint when and if a respiratory patient qualifies for hospice, but it’s vital to improve their quality of life in the final months — at times, even extending their life by several weeks.
How will you know when it’s time to call on hospice for your loved one with lung disease? What symptoms do you need to look for? Finally, what benefits does hospice provide that regular palliative care doesn’t?
Hospice Eligibility for Lung Disease
The criteria to qualify for hospice benefits are: 1) Doctors give a prognosis of six months or less and 2) The patient stops all curative treatments for an end-stage disease. For lung conditions specifically, a patient may qualify for hospice if they experience:
- Disabling shortness of breath at rest (dyspnea).
- Frequent ER visits or hospitalizations for lung infections or respiratory failure.
- Continued functional decline (bed to chair existence, fatigue, cough).
- Low levels of oxygen or high levels of carbon dioxide in the blood.
- Unintentional weight loss, >10% in 6 months.
- Advanced-stage lung cancer.
OR - The patient chooses not to pursue any further curative treatment.
Some lung conditions that can qualify for hospice eligibility include Chronic Obstructive Pulmonary Disease (COPD), Chronic Asthma, Emphysema, Bronchiectasis, Lung Cancer, Idiopathic Pulmonary Fibrosis, Sarcoidosis, Amyotrophic Lateral Sclerosis (ALS), Muscular Dystrophy, and Mechanical Lung Restriction.
End-of-life care conversations between patients, family members, caregivers, and doctors should take place when the patient shows the following signs:
- Inability to carry on any physical activity without chest pain.
- Shortness of breath while at rest/reclined.
- Increased weakness or fatigue.
- Neck vein distention.
- Weight gain secondary to edema.
- Weight loss secondary to poor nutrition.
- Increased use of oxygen.
- Increased anxiety and depression.
- Fear and anger.
- Grief and feelings of loneliness.
Hospice Benefits for Lung Conditions
It’s a common myth that hospice provides little to no care beyond pain management; a host of resources that offer comfort, education, training, and mental and emotional support for the whole family opens up once hospice benefits are applied. Plus, hospice coverage is provided by Medicare, Medicaid, VA, and health insurance plans.
On hospice, patients often spend their final months or weeks of life at home surrounded by loved ones, instead of in the hospital. Beyond a better quality of life, terminally ill patients on hospice live an average of 29 days longer than non-hospice patients. For lung cancer patients, results showed 39 days longer. These extra days of life can often bring closure, time to say goodbye, and peace to patients and their families.
Other benefits of hospice care for pulmonary patients includes:
- Lung disease education and support, including Heart to Heart Hospice’s proprietary Pulmonary Patient/Caregiver Guide and Symptom Tracking Log.
- Increased caregiver confidence and relief with volunteer visits or respite care.
- Management of a patient’s physical symptoms through medication and non-curative therapies.
- Reduction of ER visits and hospitalizations, with increased patient visits per the hospice care plan.
- A PULMONARY WARNINGS tool to identify and rapidly respond to symptom changes.
- 24/7 on-call support that can triage over the phone and determine if an in-home visit is needed.
- Emotional and spiritual support via social workers and spiritual care coordinators, with care for anxiety, depression, and fear.
- Support in making final arrangements and bereavement care for families after the patient’s death.
Heart to Heart Hospice offers Care Bridge Pulmonary Care that provides extensive training for the hospice team about respiratory diseases and lung conditions, palliative treatments (also called comfort care), optimal symptom management, and social issues that impact a patient’s mental and emotional wellbeing. Extra pulmonary therapies to control symptoms (but not extend life) are available, as well as extensive in-home caregiver training and support.
Breaking the Cycle
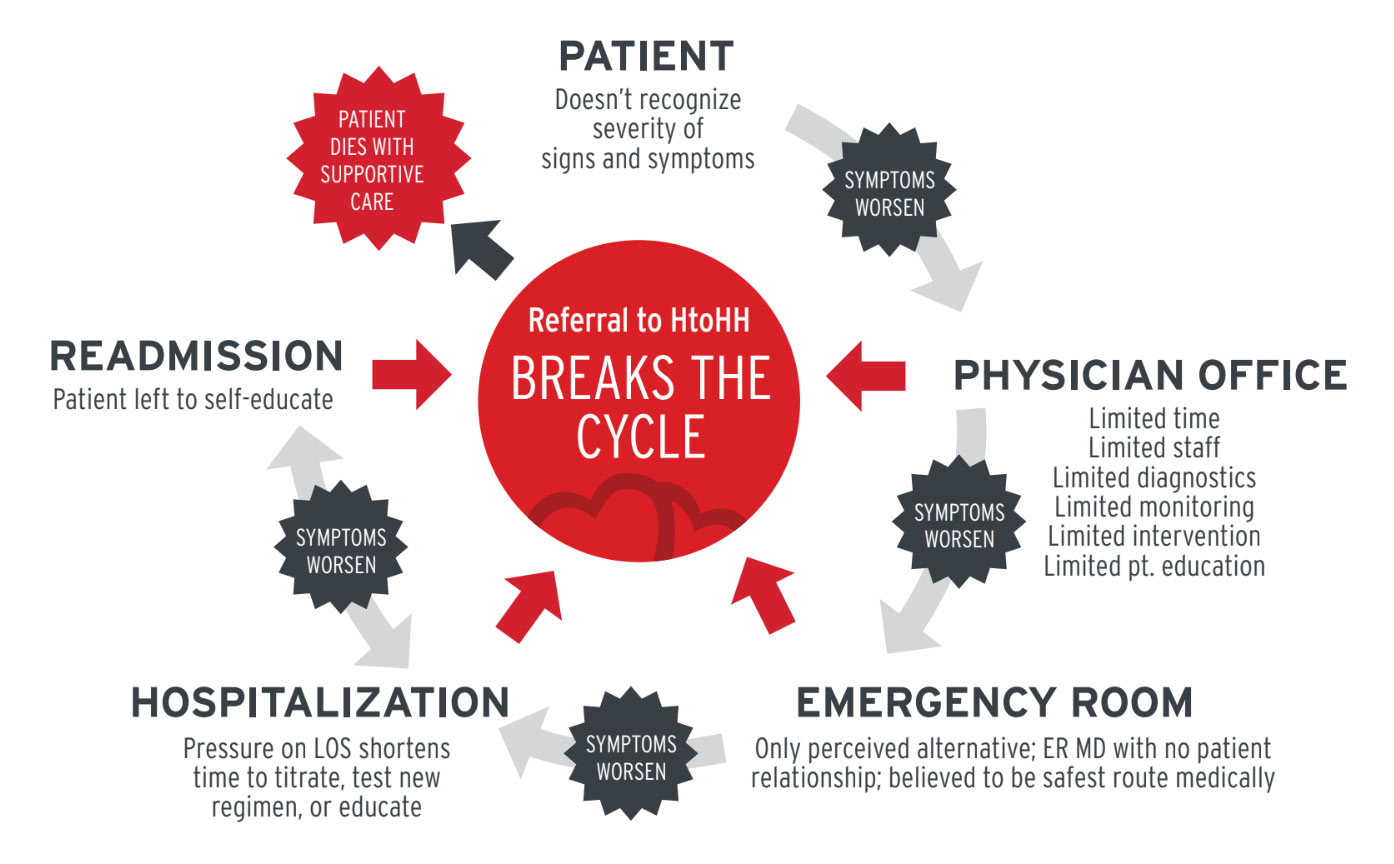
Educating healthcare professionals and facilitating important conversations with patients and families help break the cycle of constant rehospitalizations for lung patients. COPD was the third leading cause of death (pre COVID), excluding accidents, yet lung disease represents just 11% of all hospice diagnoses. Instead of constant doctor’s appointments or emergency room visits with different providers, hospice offers continuity of care that helps alleviate the burden from terminally ill patients and their families.
For patients with end-stage pulmonary diseases, Heart to Heart Hospice offers specialized care that provides comfort, support, and dignity. If you live in Indiana, Michigan, or Texas, see if there is a Heart to Heart provider in your area.

